We all at some point have that fleeting thought that randomly pops up in our heads. For instance, “Did I really lock the door before leaving? But for most of us we just brush it off and it disappears quickly. But for someone with obsessive-compulsive disorder (OCD), these thoughts do not go away quickly; they plant roots and echo louder when next it comes. These thoughts gradually develop into symptoms that, if not treated or managed interfere with relationships, work performance, academics, and even everyday functioning.
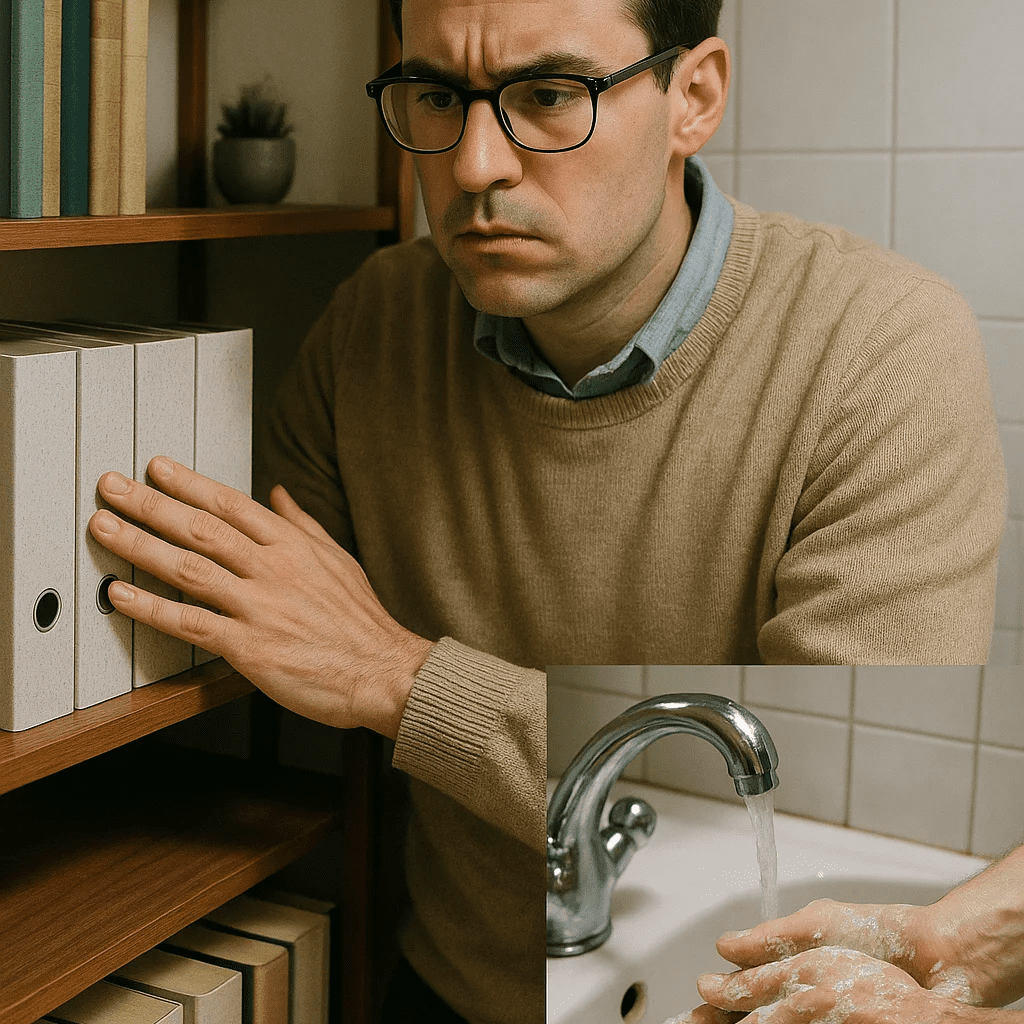
When most people hear “OCD,” they picture someone who washes their hands a lot or likes things arranged perfectly. But Obsessive-Compulsive Disorder is far more complex and much more painful than neatness or unusual habits. It is more about having no control over negative thoughts and being afraid of things going wrong if not done in a certain way.
Let us explore what OCD really feels like, how it manifests, and what science says about its causes and treatment.
What Is OCD?
Obsessive-Compulsive Disorder (OCD) is an anxiety/personality disorder that presents two main symptoms:
- Obsessions: Persistent thoughts, urges, or images in the mind that trigger distress or anxiety. They are intrusive, meaning the person cannot help having these thoughts.
- Compulsions: Repetitive actions or rituals that people feel compelled to do just to calm down the anxiety caused by the obsessions.
Example: If someone has an obsession about germs or dirt, they have the compulsion to constantly wash their hands over and over again.
In summary, people with OCD have unwanted intrusive thoughts that are always repetitive. Unlike the way some people joke about having OCD because they like things neat, perfect and in order or cannot stop thinking about something, OCD symptoms are not enjoyable and rarely bring relief. Because for someone who truly has OCD, despite knowing how irrational it is to keep worrying or doing the same thing, they just cannot help the thought.
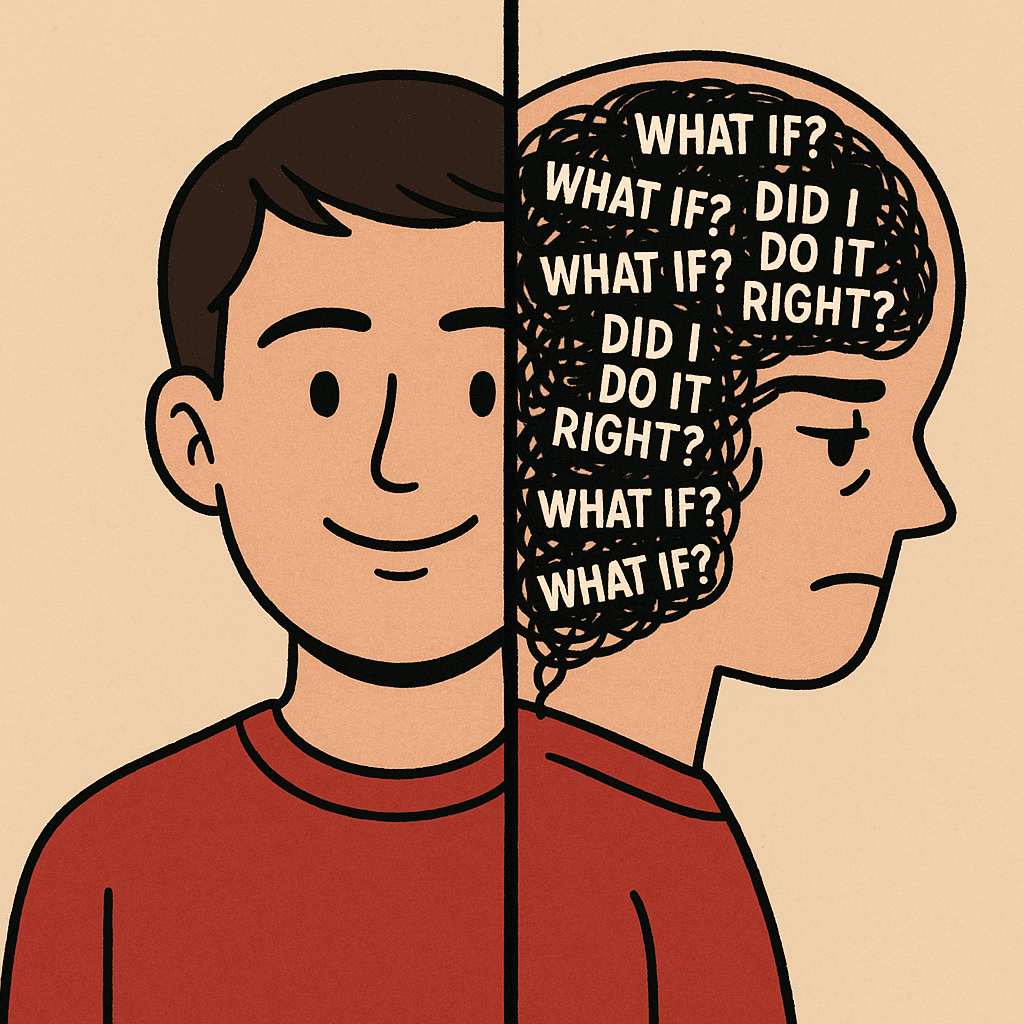
What OCD Feels Like: Inside the Mind of Someone Struggling
Imagine you turn off your gas cooker before going to work and as you step out, a voice in your head keep whispering or screaming “are you sure the gas cooker is off, if you do not go back and switch it off, there might be a fire outbreak. You go and check and find out that everything is off, but the thought keeps coming continuously. You know it does not make sense. But the fear feels real. That is the mental trap many with OCD live in every day.
Common types include:
- Contamination fears: Fear of germs, illness, or chemical exposure. For instance, people with this fear often feel the need to wash their hands over and over again, worrying that they might have missed a spot and could get sick.
- Harm obsessions: Fear of accidentally hurting others or oneself or responsible for the bad thing happening. Example, what if I cause a fire outbreak?
- Doubt and Uncertainty: People in this category are always not certain and having doubt about their actions. For instance, they might keep asking “Did I really lock the doors before leaving? even after locking their doors.
- Perfectionism: Needing things to be perfect with no mistake to prevent bad outcomes.
- Sexual or violent intrusive thoughts: These unwanted sexual thoughts that go against or do not match one’s beliefs or values, yet they keep coming. Example People with this kind of obsession can have HIV text multiple times even if there is no cause for it.
- Religious or moral obsessions: Intense fear of sinning or offending religious figures, obsessing over morality.
For someone, you can be having just one of these obsessions, two or even more. I hope you are beginning to realise your own.
What Causes OCD? Brain, Biology & Beyond
The root causes of OCD involve a complex interaction between genetics, brain chemistry, and life experiences with:
- Brain structure and function: People with OCD often have differences in how certain parts of their brain work, especially areas that deal with decision-making, worry, and habit formation.
- Genetic predisposition: If someone in your family has OCD, you’re more likely to develop it too. This does not mean you are guaranteed to get it, but the risk goes up. Twin and family studies show that OCD has a strong genetic component. For example, if an identical twin has OCD, the other twin is more likely to have it too.
- Environmental triggers: Traumatic events, childhood abuse, or chronic stress can trigger or exacerbate symptoms.
💡 Diagnosing OCD
Health practitioners usually misdiagnosed OCD or do not diagnose it at all. Most people hide their symptoms because of fear or the stigma that comes along with it. This results in a delayed effective treatment. The World Health Organization ranks OCD among the top 10 most disabling illnesses in terms of lost income and decreased quality of life (Veale & Roberts, 2014).
Accurate diagnoses include:
- A mental health professional’s assessment: While there is no single test for the disorder because symptoms can be related to those of a personality disorder, anxiety disorders, depression, or other mental health disorders. Diagnosis of the disorder is typically made up of assessment such as evaluating a person’s symptoms, mental health history and how much the obsessions and compulsions impact their daily life.
- Use of instruments such as the Yale-Brown Obsessive Compulsive Scale (Y-BOCS).
How Is OCD Treated?
Fortunately, OCD is treatable, even if it does not result in a cure, the symptoms can be brought under control with the right interventions:
🔹 Cognitive-Behavioural Therapy (CBT)
More specifically, Exposure and Response Prevention (ERP) is one of the most effective treatments for OCD. This involves exposing oneself to what triggers the anxiety yet not performing the ritual behaviours that help calm down these anxieties. For instance, if your compulsion is to continuously wash your hands, you start by limiting the number of times you do so despite the doubt.
🔹 Medication
There are medications prescribed according to age, example: some for adult and children, adult only or children only. Some medications are also given according to age for instance 7 years and above, 10 years and above etc. Common among them is Selective Serotonin Reuptake Inhibitors (SSRIs), such as fluoxetine and sertraline, are typically prescribed.
However, your doctor is more cable of prescribing other antidepressants and psychiatric medicines.
🔹 Lifestyle & Support
- You must be mindful of yourself and accept that you have a disorder.
- Joining a support group or community (e.g., via the International OCD Foundation) helps reduce isolation.
- Regular sleep routine, proper nutrition, and regular exercise helps contribute to emotional resilience.
Myths That Need Busting
Let’s clear up a few common misconceptions:
❌ OCD is just about being clean or organised.
✅ OCD is about anxiety-driven compulsions, often unrelated to cleanliness.
❌ People with OCD enjoy their rituals.
✅ They feel compelled to do them, often with distress and reluctance.
❌ You can “just stop” doing compulsions.
✅ OCD involves deeply rooted neurological and psychological mechanisms. Recovery takes time and support.
Living With OCD: A Journey of Courage
Having OCD does not mean giving up on dreams, relationships, or happiness. It means learning to work in harmony with your mind, instead of against it. OCD is not something you wish to have or something you joke about having, it is a serious mental illness that deserves to be understood and sensitively appreciated. With early intervention, ongoing support, and compassionate care, people with OCD are able to lead full, satisfying lives.
By acknowledging the science, welcoming the experience, and promoting evidence-based practice, we move one step further to shatter the stigma. Should you or anyone you know be struggling, know that you’re not alone and assistance is available.



This article is so amazing and educative, our mental health should be our priority because A HEALTHY MIND IS A HEALTHY BODY.
[…] Obsessive compulsive disorder […]