Imagine you’re driving and hear a loud bang. Your heart races, palms sweat, and you tense up — just like you did during a traumatic event years ago. For someone with PTSD, everyday triggers can ignite a storm of intense fear and distress.
Post-Traumatic Stress Disorder is not a character flaw or weakness — it’s a physiological response to overwhelming stress that changes the brain itself. Today, we’ll unpack the science of PTSD, explore which parts of the brain it affects, and show why healing is absolutely possible.
What is PTSD?
Post-Traumatic Stress Disorder (PTSD) is a psychiatric condition arising after witnessing or experiencing terrifying events.
According to the National Institute of Mental Health (NIMH), about 6% of U.S. adults will experience PTSD at some point in their lives (source).
Common Symptoms:
- Reliving trauma through flashbacks or nightmares.
- Avoidance of people, places, or things that remind them of the trauma.
- Persistent negative emotions like fear, anger, guilt, or shame.
- Hyperarousal symptoms like difficulty sleeping, irritability, and being easily startled.
There’s no one-size-fits-all cause — from car accidents and abuse to military combat and natural disasters.
What’s consistent is that PTSD fundamentally alters how the brain processes fear, memory, and safety.
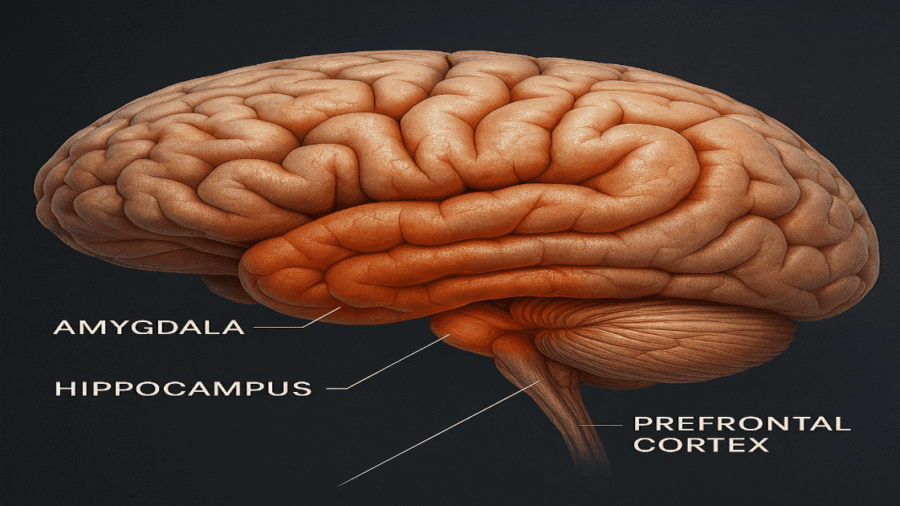
Key Brain Structures Affected by PTSD
Let’s break down the three main players altered by PTSD:
1. The Amygdala: The Fear Factory
The amygdala is your brain’s alarm bell — critical for detecting danger and setting off a quick survival response.
In PTSD:
- The amygdala becomes hypersensitive.
- It overreacts to perceived threats, even if they’re harmless (like a car backfiring or a crowded room) (source: NIH).
For instance, A war veteran may drop to the ground when hearing fireworks — the amygdala mistakenly signals that the individual is under attack.
Brain imaging studies have consistently shown increased amygdala activity in PTSD patients.
2. The Hippocampus: Memory and Context Gatekeeper
The hippocampus helps us differentiate between safe and dangerous environments and puts memories into context.
In PTSD:
- It shrinks (reduced volume by up to 8%, according to MRI studies).
- It misfiles memories, leading to vivid, emotionally-charged recollections that feel like current experiences instead of past ones.
A survivor of a house fire might smell smoke from a BBQ and instantly be thrust back into terror, unable to distinguish the safe BBQ from the deadly fire.
A 2007 review in Neuroscience & Biobehavioral Reviews concluded hippocampal volume loss is a hallmark of PTSD.
3. The Prefrontal Cortex: The Rational Regulator
The prefrontal cortex governs rational thinking, impulse control, and emotional regulation.
In PTSD:
- It loses activity (“hypoactivation”).
- It fails to inhibit the overactive amygdala.
- Emotional responses override logical thought.
Example:
Someone with PTSD may know intellectually that they are safe at a party, but still feel trapped, panicked, and desperate to escape.
fMRI scans show that individuals with PTSD often exhibit reduced blood flow and activity in the medial prefrontal cortex.
Neurochemical Changes in PTSD
Beyond structural shifts, PTSD deeply disrupts brain chemistry:
Key Neurochemical Shifts:
- Cortisol: The hormone meant to regulate stress becomes unstable. In PTSD, cortisol levels may be unusually low, leading to poor control over stress reactions.
- Norepinephrine: Elevated levels cause constant hypervigilance — making sufferers jumpy, irritable, and unable to relax.
- Serotonin: This “feel-good” neurotransmitter drops, contributing to depression, anxiety, and emotional numbness(source: Harvard Health).
Impact:
These chemical imbalances reinforce the brain’s threat response, creating a vicious cycle where the body remains “stuck” in trauma even long after the event.
Research from Biological Psychiatry emphasizes the role of neurotransmitter imbalance in PTSD development and maintenance.
Functional Brain Changes
PTSD isn’t just structural or chemical — it changes how the brain functions day-to-day.
1. Hyperarousal
- Constant readiness for danger.
- Symptoms: Insomnia, exaggerated startle response, irritability.
2. Intrusive Memories and Flashbacks
- Triggered by sensory reminders (smells, sounds).
- Memories are relived, not just remembered.
3. Emotional Numbing and Dissociation
- A coping strategy where emotions are “shut off.”
- Sufferers may feel detached from themselves or their surroundings (like living in a fog).
Dissociative symptoms correlate with abnormal activation in the default mode network (DMN) of the brain.
Can the Brain Heal from PTSD?
Absolutely.
Thanks to neuroplasticity, the brain can forge new pathways and heal old wounds.
Evidence-Based Treatments That Promote Healing:
- Psychotherapy:
- Cognitive Behavioral Therapy (CBT): Reduces distorted thinking.
- Eye Movement Desensitization and Reprocessing (EMDR): Helps reprocess traumatic memories in a safer context.
- Medication:
- SSRIs like sertraline and paroxetine help regulate mood and anxiety.
- Emerging Options:
- MDMA-assisted psychotherapy is showing an astounding 67% remission rate in Phase 3 clinical trials.
Lifestyle Supports:
Mindfulness, yoga, and even journaling help rebuild neural connections and decrease amygdala overactivity over time.
FAQs About PTSD and the Brain
Does PTSD cause permanent brain damage?
Not usually. While changes can be long-lasting, the brain’s plasticity allows significant recovery through therapy and supportive care.
How does PTSD rewire the brain?
PTSD strengthens fear networks (amygdala) and weakens safety networks (prefrontal cortex and hippocampus).
Can therapy reverse PTSD-related brain changes?
Yes. Studies show that successful treatment correlates with normalized brain structure and function.
What happens to the brain during a PTSD flashback?
The brain relives trauma by hyperactivating the amygdala while the hippocampus fails to distinguish memory from present reality.
Real-Life Implications and Takeaways
Understanding the biology of PTSD helps shift the conversation:
👉 It’s not a moral weakness.
👉 It’s a neurobiological injury.
Early intervention, compassion, and consistent treatment can literally rewire the brain for healing.
Conclusion
PTSD fundamentally changes how the brain perceives and reacts to the world — but it doesn’t have to be permanent.
Thanks to advances in neuroscience, we now know that the brain can recover, adapt, and even grow stronger.
If you or someone you love struggles with PTSD, remember:
Healing is not only possible — it’s backed by science.


Add a Comment